If You’re Worried About LDL Cholesterol, You’re Looking in the Wrong Place
Introduction: Why LDL Became the Scapegoat
If you’ve ever had blood work flagged for “high LDL cholesterol,” you were likely told one thing: Lower it.
Lower it with diet.
Lower it with medication.
Lower it as fast as possible.
But LDL cholesterol does not operate in isolation.
LDL is not inherently dangerous. It becomes problematic only within a hostile biological environment. Cardiovascular risk is not driven by a single number — it’s driven by the terrain LDL particles are exposed to.
LDL Is a Transport Molecule, Not a Villain
LDL particles transport:
cholesterol
fat-soluble vitamins
repair materials
They exist to support cellular function.
LDL only contributes to disease when:
Inflammation is high
Insulin resistance is present
Blood vessels are damaged
Oxidative stress is excessive
In healthy terrain, LDL does its job quietly and efficiently.
The Real Risk Framework (What Matters More Than LDL)
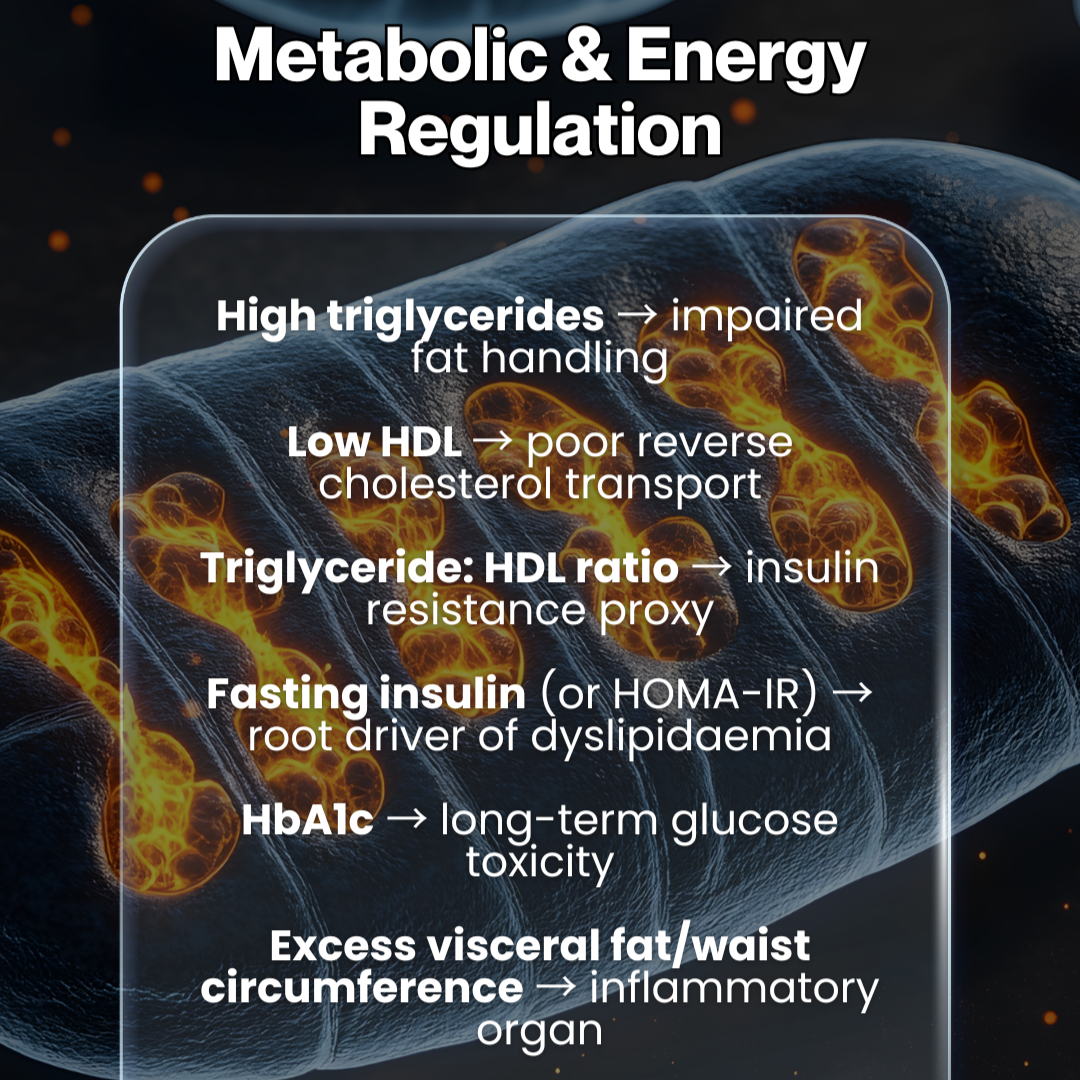
1. Metabolic & Energy Regulation
Poor metabolic health forces lipids to behave badly.
Key markers that matter more than LDL-C alone:
High triglycerides → impaired fat handling
Low HDL → poor reverse cholesterol transport
Triglyceride: HDL ratio → a strong insulin resistance proxy
Fasting insulin / HOMA-IR → upstream dyslipidaemia driver
HbA1c → long-term glucose toxicity
Excess visceral fat → inflammatory organ, not storage tissue
If insulin resistance is present, LDL is being pushed into a system that cannot process it safely.
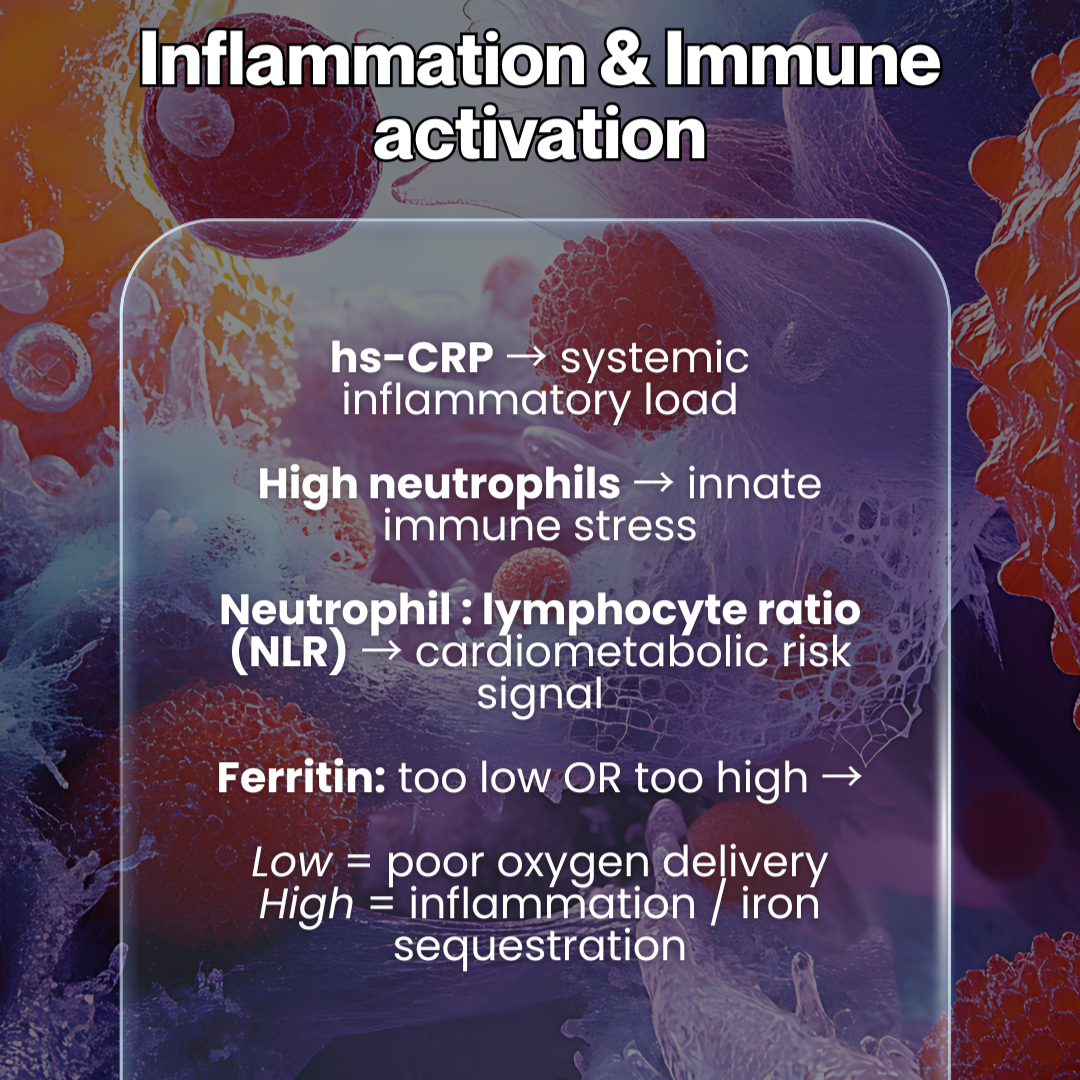
2. Inflammation & Immune Activation
LDL becomes dangerous only after inflammation is established.
Markers that signal true risk:
hs-CRP → systemic inflammation
High neutrophils → innate immune stress
Neutrophil: lymphocyte ratio (NLR) → cardiometabolic risk signal
Ferritin too low OR too high
Low → impaired oxygen delivery
High → inflammation and iron sequestration
Inflammation oxidises LDL. Oxidised LDL is what damages tissue — not LDL itself.
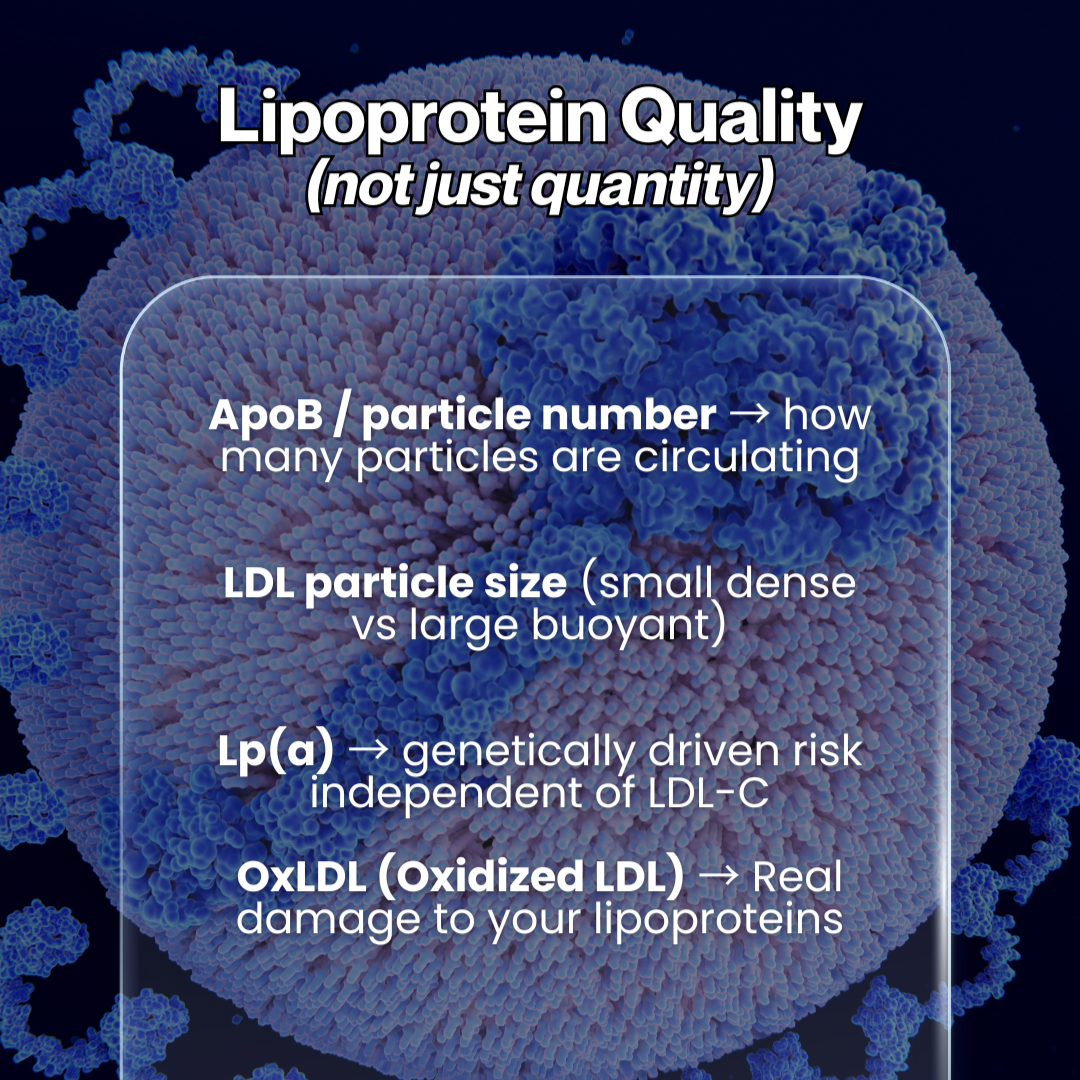
3. Lipoprotein Quality (Not Just Quantity)
Two people can have the same LDL-C level and yet have completely different risk profiles.
What actually matters:
ApoB / particle number → how many particles are circulating
LDL particle size → small dense vs large buoyant
Lp(a) → genetically driven risk independent of LDL-C
OxLDL → true oxidative damage marker
This explains why LDL-C alone is a poor predictor of outcomes.
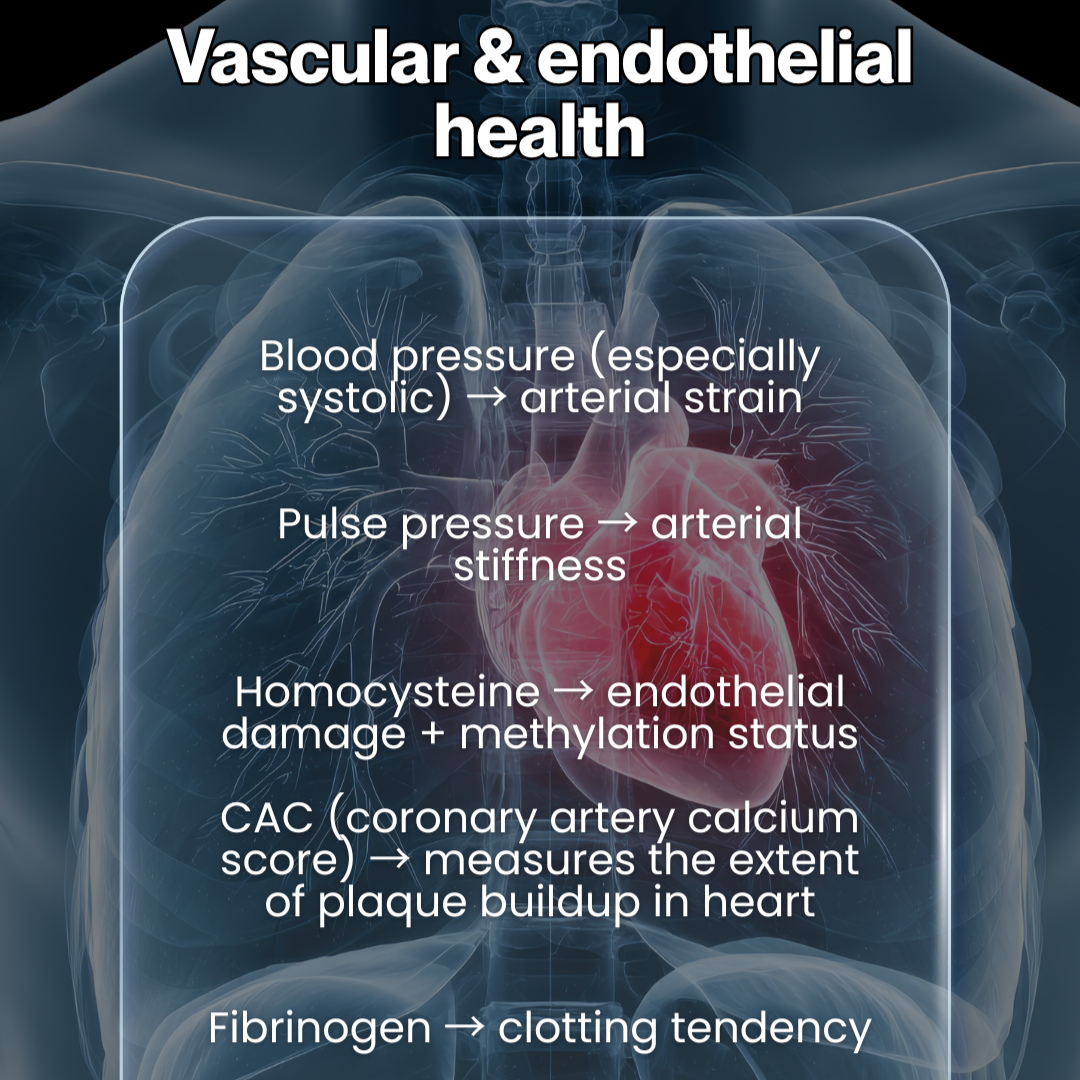
4. Vascular & Endothelial Health
Plaque forms where vessels are already injured.
Key indicators:
Blood pressure (especially systolic) → arterial strain
Pulse pressure → arterial stiffness
Homocysteine → endothelial damage + methylation status
CAC score → actual plaque burden
Fibrinogen → clotting tendency
Healthy endothelium resists plaque formation — even with elevated LDL. Read more about the connective tissue with the glycocalyx, and how it can set the stage for plaque formation in my article HERE.
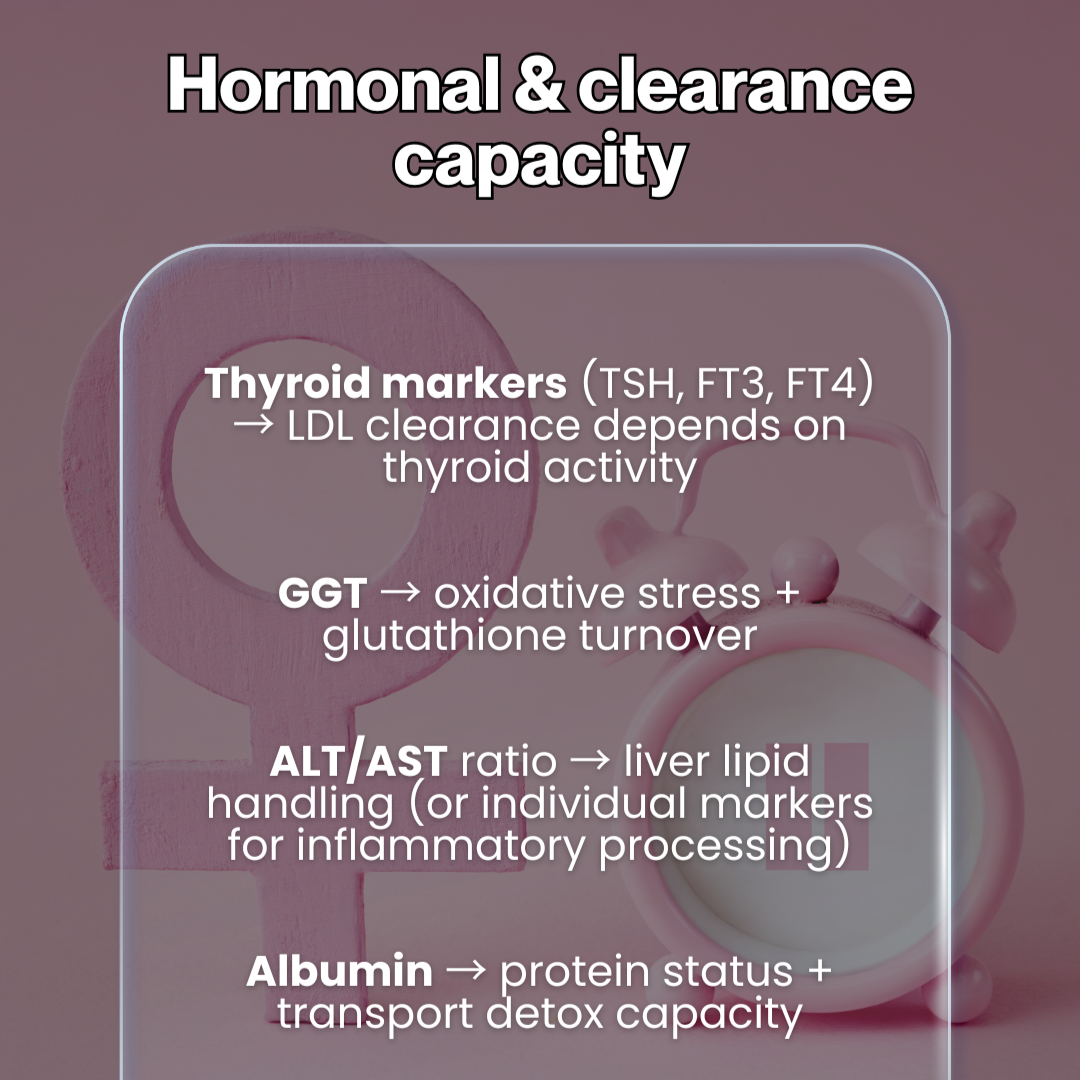
5. Hormonal & Clearance Capacity
LDL clearance depends on liver, thyroid, and gut function.
Critical markers:
Thyroid hormones (TSH, FT3, FT4) → LDL receptor activity
GGT → oxidative stress + glutathione demand
ALT : AST ratio → liver lipid handling
Albumin → protein status + detox transport
When clearance is impaired, LDL accumulates regardless of intake.
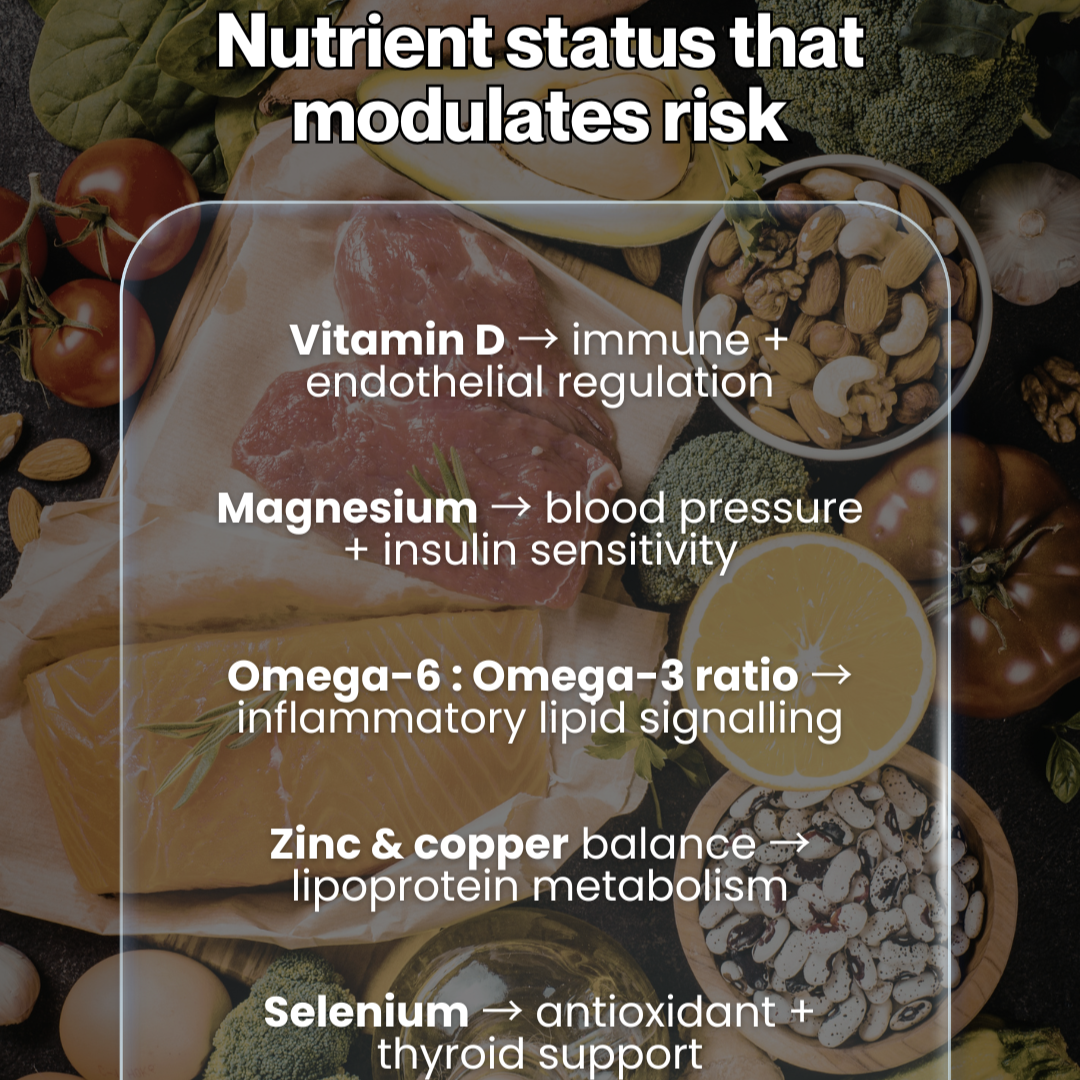
6. Nutrient Status That Modulates Risk
Deficiencies alter lipid behaviour:
Vitamin D → immune + endothelial regulation
Magnesium → insulin sensitivity + blood pressure
Omega-6 : Omega-3 ratio → inflammatory lipid signalling
Zinc & copper balance → lipoprotein metabolism
Selenium → antioxidant defence + thyroid support
Vitamin E → Depending on your PUFA intake and oxidative stress.
Nutrient-deficient systems turn neutral particles reactive.
7. Lifestyle Context (The Silent Amplifier)
No marker exists in a vacuum. Risk escalates with:
poor sleep timing and duration
chronic psychological stress
smoking or vaping
physical inactivity
chronic calorie restriction
Lifestyle creates the environment LDL responds to.
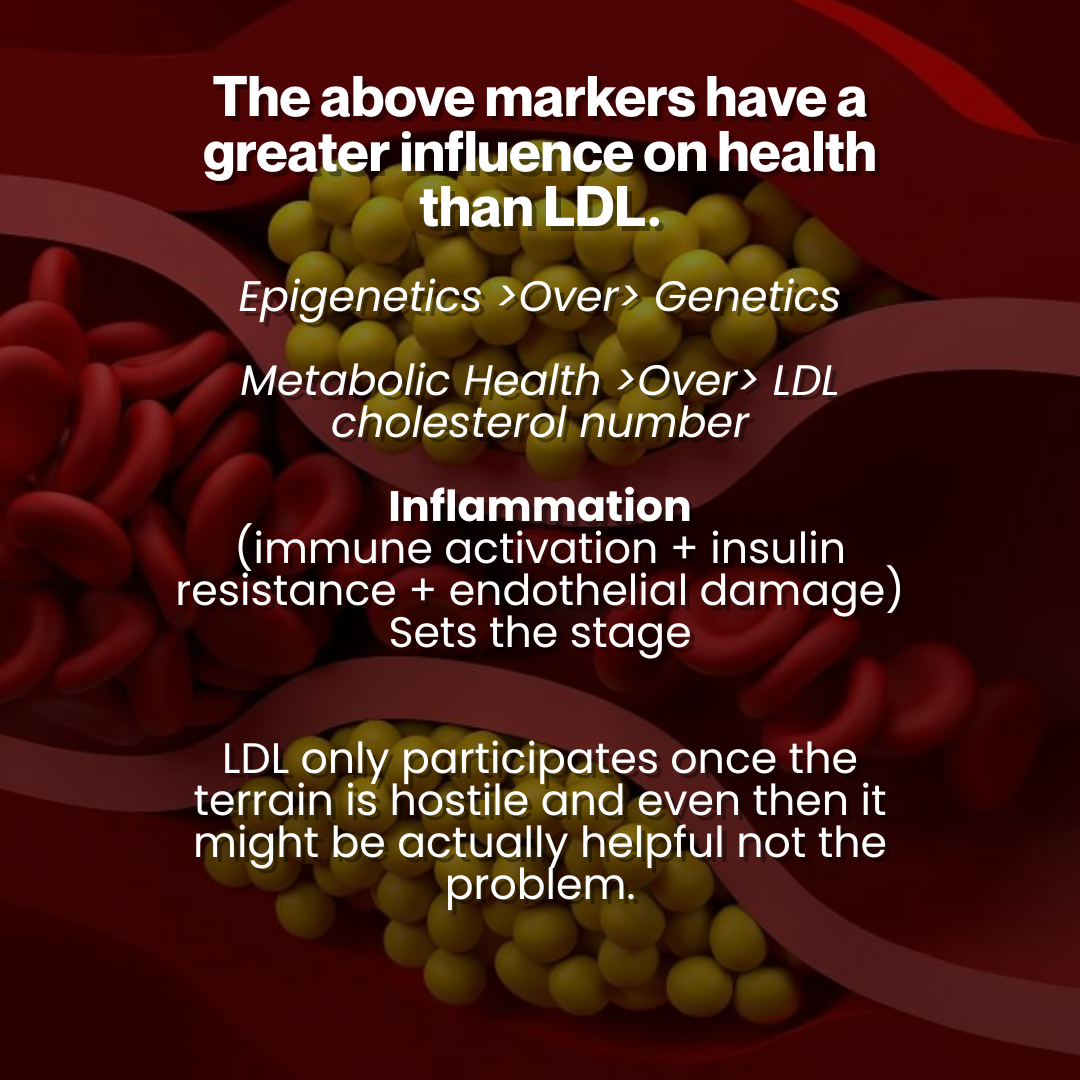
The Honest Hierarchy of Risk
Inflammation, insulin resistance, immune activation, and endothelial damage set the stage.
LDL only participates once that terrain becomes hostile. But even then, the act of wanting to lower it via medication such as a statin results in a mediocre performance when, instead, optimising nutritional factors above and positively influencing the microbiome can make massive improvements.
Lowering LDL without fixing the terrain is not preventative medicine. It is cosmetic risk management.
Final Takeaway
If you’re worried about LDL cholesterol, ask better questions:
Is inflammation low? Gut health matters.
Is insulin under control? Junk food and junk light.
Are blood vessels healthy? Movement + Sunlight + Collagen intake.
Is lipid clearance working? Bile flow + Microbiome + Bowel movements.
Fix the system — and the numbers follow.